In recent months, Canada has witnessed an alarming rise in measles infections, raising concerns about the state of public health and vaccine confidence across the nation. Morgan Birch, an Alberta mother, first identified her four-month-old daughter Kimie's illness as measles—a sickness most Canadians thought had been eradicated since 1998. With over 3,800 Canadians infected in 2025, Canada has become the center of a measles outbreak, outpacing the U.S., which has seen significantly fewer cases.
Health authorities have attributed the crisis primarily to a decline in vaccination rates, exacerbated by the effects of misinformation regarding vaccines, particularly among conservative Mennonite communities where cultural beliefs often discourage immunization. These communities have become breeding grounds for the virus due to their historical resistance to vaccines, further fueled by a wave of anti-vaccine sentiments post-COVID-19.
Catalina Friesen, a healthcare worker servicing a Mennonite area in southern Ontario, marked the community's first encounter with measles. The outbreak began when the virus was transmitted at a large Mennonite gathering and swiftly spread among unvaccinated individuals. Reports indicate that the majority of infected individuals had not received the measles, mumps, and rubella (MMR) vaccine.
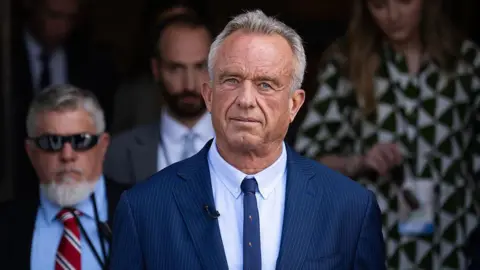
Unlike the U.S., which has attributed some of its outbreak to high-profile vaccine-hesitant figures, Canada's health discourse does not feature similar prominent individuals, perhaps complicating understanding of the outbreak's causes. Postdoctoral public health fellow Maxwell Smith noted that the Canadian context, which includes a lack of strong pro-immunization advocacy, likely plays a role in this ongoing crisis.
The challenge remains significant. Reports indicate a drastic decline in MMR vaccinations since 2019, down by nearly half in some regions, often stemming from public skepticism surrounding vaccine mandates. The recent decline in routine immunizations during the pandemic has further compounded the issue, as families prioritize other vaccinations over measles due to its past elimination.
Public health initiatives are underway, emphasizing the importance of vaccines to curb the outbreak's rampant spread. Yet the response has been tepid compared to the mass mobilization witnessed during COVID-19 vaccination campaigns. Meanwhile, as the consequences of this outbreak unfold, families like that of Morgan Birch are left grappling with the ramifications of this preventable disease, calling for greater adherence to public health guidance to fortify community immunity and protect those unable to vaccinate.
Health authorities have attributed the crisis primarily to a decline in vaccination rates, exacerbated by the effects of misinformation regarding vaccines, particularly among conservative Mennonite communities where cultural beliefs often discourage immunization. These communities have become breeding grounds for the virus due to their historical resistance to vaccines, further fueled by a wave of anti-vaccine sentiments post-COVID-19.
Catalina Friesen, a healthcare worker servicing a Mennonite area in southern Ontario, marked the community's first encounter with measles. The outbreak began when the virus was transmitted at a large Mennonite gathering and swiftly spread among unvaccinated individuals. Reports indicate that the majority of infected individuals had not received the measles, mumps, and rubella (MMR) vaccine.
Unlike the U.S., which has attributed some of its outbreak to high-profile vaccine-hesitant figures, Canada's health discourse does not feature similar prominent individuals, perhaps complicating understanding of the outbreak's causes. Postdoctoral public health fellow Maxwell Smith noted that the Canadian context, which includes a lack of strong pro-immunization advocacy, likely plays a role in this ongoing crisis.
The challenge remains significant. Reports indicate a drastic decline in MMR vaccinations since 2019, down by nearly half in some regions, often stemming from public skepticism surrounding vaccine mandates. The recent decline in routine immunizations during the pandemic has further compounded the issue, as families prioritize other vaccinations over measles due to its past elimination.
Public health initiatives are underway, emphasizing the importance of vaccines to curb the outbreak's rampant spread. Yet the response has been tepid compared to the mass mobilization witnessed during COVID-19 vaccination campaigns. Meanwhile, as the consequences of this outbreak unfold, families like that of Morgan Birch are left grappling with the ramifications of this preventable disease, calling for greater adherence to public health guidance to fortify community immunity and protect those unable to vaccinate.